The Hospital Industry and Workforce Update – Before and After the Pandemic Recession
December 13, 2023The hospital industry is a sub-sector of the one of the largest industries in the nation – the health care and social assistance sector. National employment in the health care and social assistance industry reached 22.9 million in March 2023 and made up 15.1% of total industry employment. The nation’s hospital industry made up 29% of the health care and social assistance industry employing 6.65 million workers in March 2023.
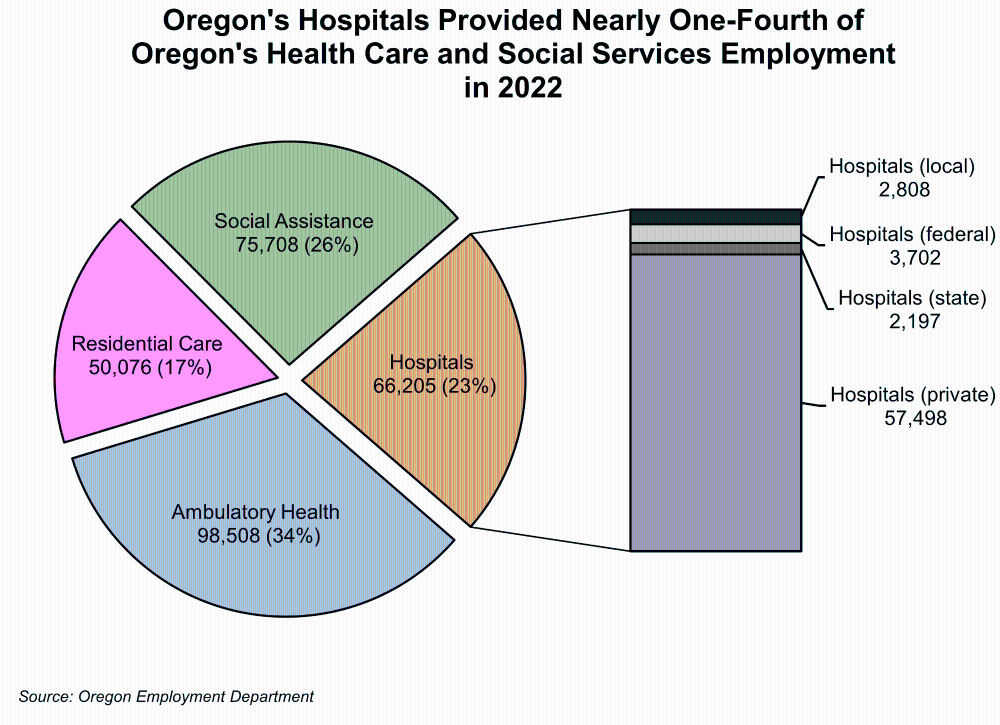
Oregon’s hospital industry made up 23% of employment in the state’s health care and social assistance sector employing 290,495 workers with a payroll of $18.4 billion in 2022. The hospital industry is made up of four ownerships – private, local, state, and federal government. In 2022, Oregon’s hospital industry (all ownerships) employed 66,205 workers with a payroll of $5.9 billion. The majority of Oregon’s hospitals are privately owned (87%) with the remaining hospitals run by local government (4.2%), federal government (5.6%), and state government (3.3%).
Higher Demand but Lower Supply of Workers
Even though Oregon’s economy is continuing to recover the jobs lost during the initial pandemic recession and has regained 86% of jobs lost in spring 2020, the number of job openings is greater than the labor force available to fill them in a number of industries. According to the Oregon Employment Department’s 2023 Winter Quarterly Job Vacancy Survey, the number of job vacancies reached record levels at 74,900 and 63% of vacancies were reported as difficult to fill. The health care and social assistance sector reported the highest vacancies of any industry at 16,451.
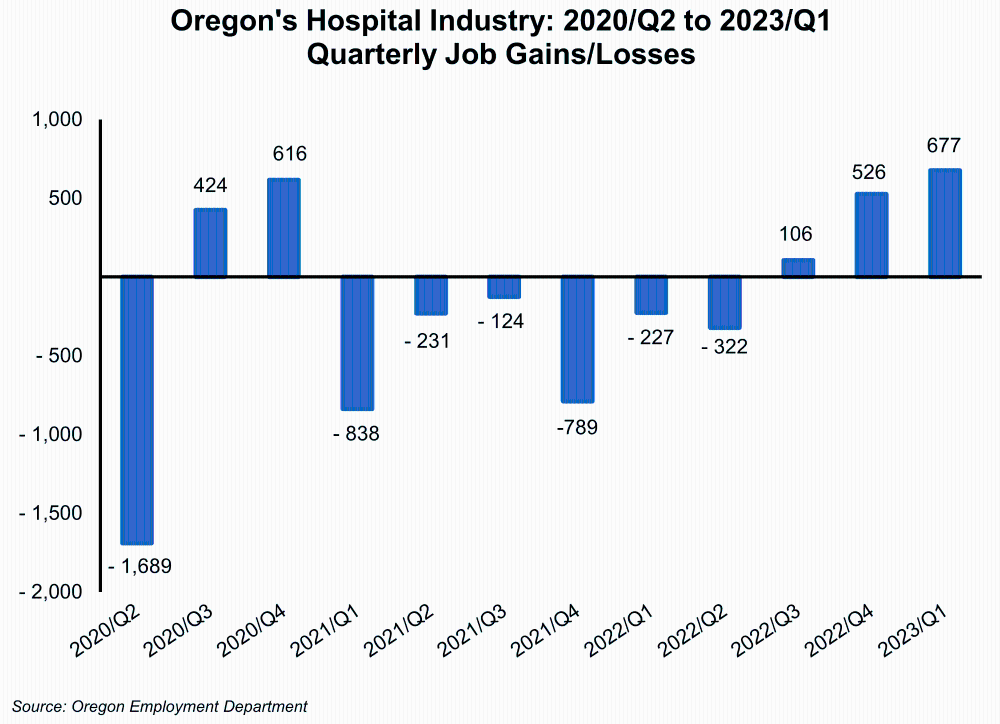
In the second quarter of 2020, Oregon’s hospital industry (all ownerships) shed 1,689 jobs. During the last two quarters of 2020, the industry added a net total of 1,040 jobs but then continued to lose more jobs than it added, with 2,531 total jobs lost from first quarter 2021 through second quarter 2022. As of first quarter 2023, employment in hospitals was 2.1% below its average level just prior to the pandemic in 2019.
Three Years After the Pandemic
Before the COVID pandemic, there were 74,263 workers in Oregon whose industry of highest earnings was the hospital industry. Of those, only 44,456 were still employed by hospitals in Oregon as of first quarter 2023 – three years later. To compare what retention looks like in any given year, the first quarter 2020 cohort of the hospital industry was examined. Three years later (2023/Q1), only 60% of this 2020 cohort remained employed in a hospital setting. So where did the former hospital workers go?
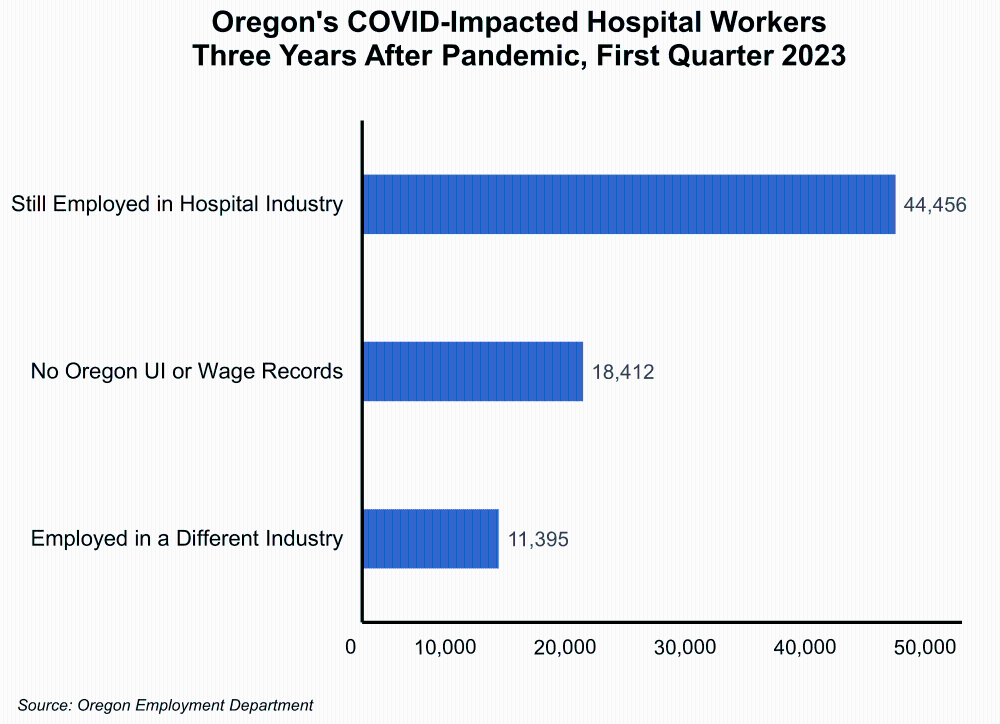
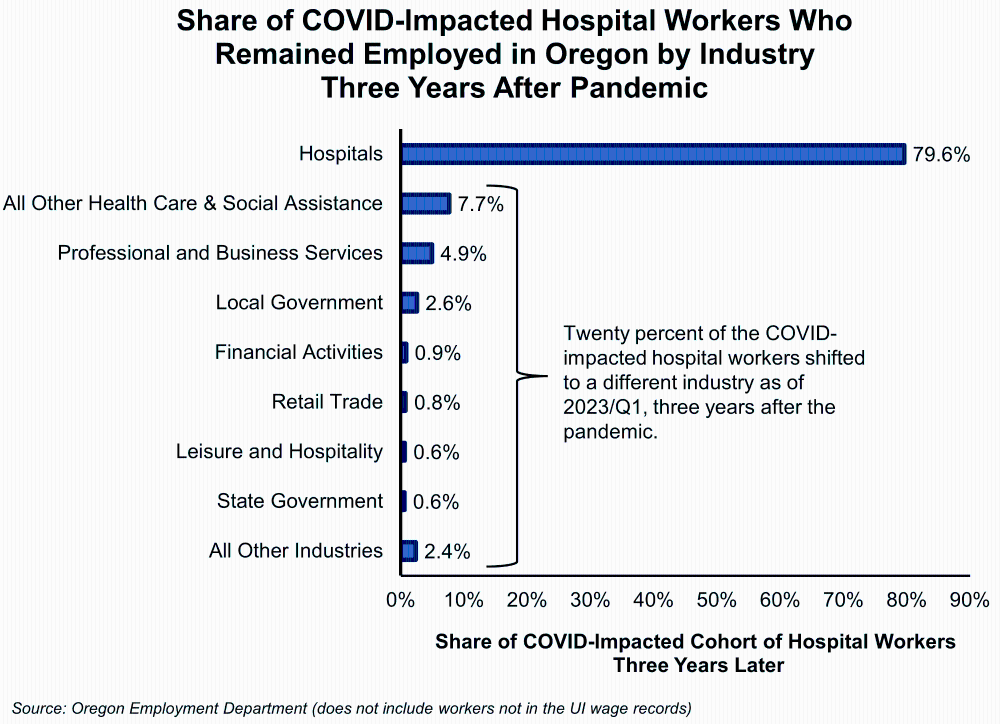
The analysis showed that 20.4% or 11,395 hospital workers who remained employed in Oregon in 2023/Q1 shifted their industry of highest earnings to a different industry. The largest shares moved to other health care and social services (7.7%); professional and business services (4.9%); and local government (2.6%). There could be numerous reasons for hospital workers to change their industry of employment during the heavy throws of the COVID pandemic and after. Some of the reasons cited by the Becker’s Hospital Review included insufficient pay or opportunities, burnout, overwork, and COVID-19 safety concerns.
Typical Occupations in the Hospital Industry
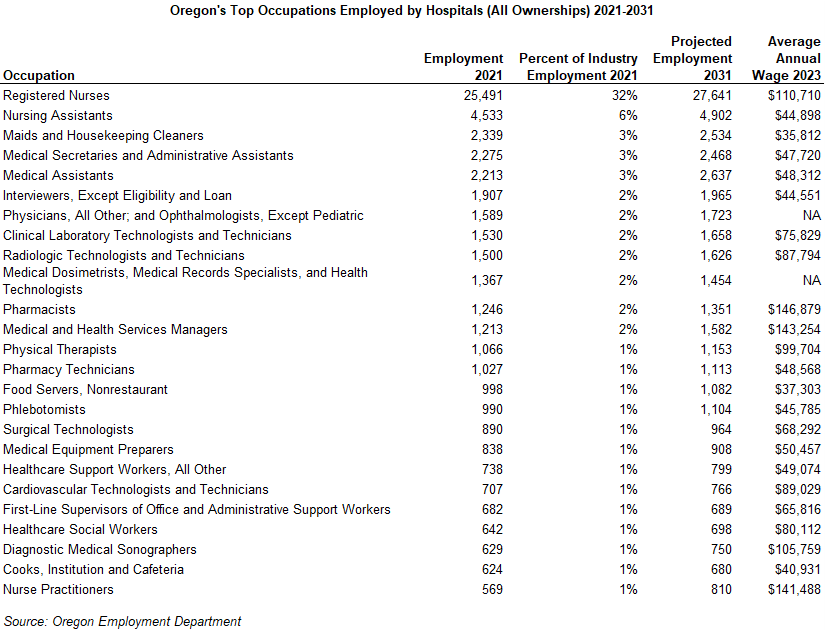
Workers from many types of occupations and with various types of skills work in hospitals, from health care professionals to office workers, food services, housekeeping, and grounds keeping and maintenance. In Oregon, the largest occupation in hospitals during 2021 was registered nurses who made up nearly one-third of the industry’s employment. The next largest occupations were nursing assistants (6%), maids and housekeeping (3%), medical secretaries (3%), medical assistants (3%), interviewers (2%), and physicians (2%).
Current Industry News
As stated in the American Hospital Association’s 2023 Fast Fact Sheet, there were 6,129 hospitals in the nation during 2023 with a total of 919,649 staffed beds. The majority (84%) of the hospitals are classified as community hospitals with 65% located in urban areas and 35% in rural areas. Community hospitals are defined as all nonfederal, short-term general, and other special hospitals.
Health care services is but one role that hospitals play in their communities. They also provide economic stability by creating jobs and purchasing goods and services from others in their communities. According to the AHA, hospitals in the U.S. supported 17.6 million jobs (one out of eight jobs in the nation) and supported $3.6 trillion in economic activity in 2020.
In a recent article in Healthcare Dive, Where are all the nurses? Hospitals, advocates disagree on crisis, there is agreement between nurses and hospital administrators that there is a nursing shortage in hospitals but no agreement on why there are so few job applicants, a lack of qualified applicants, or a lack of interest. Tension between both sides is contributing to staff authorizing strikes at numerous hospitals in the nation. During 2023, there were a number of hospitals in Oregon whose nurses and other healthcare staff voted to authorize strikes or actually ended up on the picket lines.
According to the Bureau of Labor Statistics, healthcare organization in the U.S. will need to fill nearly 200,000 open nursing positions every year until 2030. The aging nursing population who will be retiring over the next two decades will contribute to a large portion of the staffing shortages. A survey from the National Council of State Boards of Nursing showed that the average age of a registered nurse in the U.S. was 46 years old in 2022, down from 51 years old in 2020.
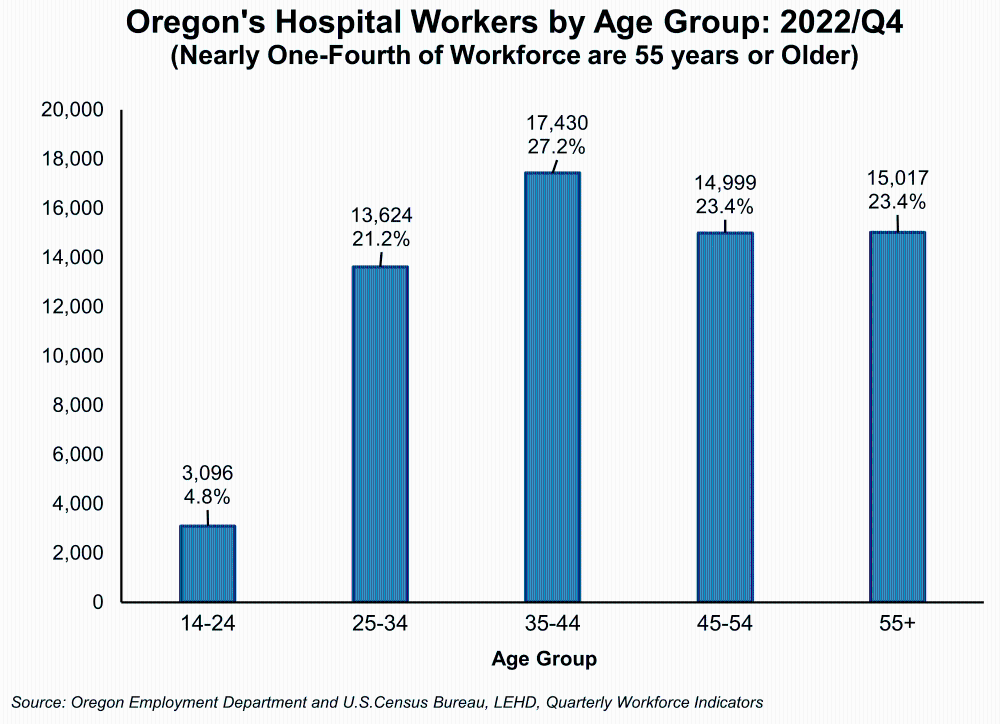
The aging of the workforce is also apparent in Oregon’s hospital industry. In the fourth quarter of 2022, nearly one-fourth of hospital workers (all occupations) were 55 years or older and another 23% were 45-54 years. In an attempt to increase the supply of nurses in Oregon, House Bill 4003 was introduced in the 2022 legislative session and eventually signed into law. This bill increases the scope of nonresident emergency nursing licenses, increases access to mental health supports, and creates new internship licenses to allow more entryways in the workforce for student nurses.
Although the race to retain and attract an adequate and talented workforce is intensifying, hopefully emerging technologies such as artificial intelligence to augment healthcare delivery and an emphasis on improving conditions for healthcare providers will help to mitigate the impending shortage.
According to an article What’s in store for healthcare in 2024, next year will see a greater focus on artificial intelligence and how hospitals will regulate and implement this new technology. More future trends in the industry can be found in the American Hospital Association’s 2024 Environmental Scan report which explores recent data and changes in the hospital industry.